Engineers Offer DIY Solutions to Coronavirus Equipment Shortages
The globe is in determined require of protecting gear to continue to keep wellness treatment employees safe and sound and ventilators to help seriously unwell COVID-19 clients breathe. In the encounter of massively elevated need and stalled offer chains, engineers are scrambling to redesign equipment so it can be produced exterior of specialised factories.
Scientists at educational institutions are drawing on the spirit of the independent maker movement, in accordance to Saad Bhamla, a bioengineer at the Georgia Institute of Engineering. “We’re tapping into this full current group,” he says, noting that numerous towns have clubs for Do-it-yourself enthusiasts. This kind of persons normally volunteer their time at fabrication labs and maker areas. Now the COVID-19 pandemic is presenting them with a special issue. “People have a connect with to arms,” Bhamla says, “and they are tapping their artistic and issue-fixing skills.”
The do-it-you method is most evident in the situation of encounter masks: hobbyists are sharing types and guidelines that allow amateurs to sew their have washable coverings. Some are donating these masks to hospitals, although in a healthcare setting, this sort of unofficial gear can only provide as a past vacation resort. Preceding investigation has revealed that when homemade facial protections can reduce the unfold of microbes, they are less productive than professionally produced surgical masks. This disparity is in component since surgical masks are manufactured from components that are greater at halting the virus-carrying droplets that spray out when humans sneeze and cough than fabrics this sort of as cotton, which is utilised in numerous homemade versions. Instead of relying on contributions from persons, some hospitals are sending healthcare-quality components to a range of apparel manufacturers, from manner designer Christian Siriano to an Amish group in Ohio, who have started mass-generating much more impermeable masks and gowns.
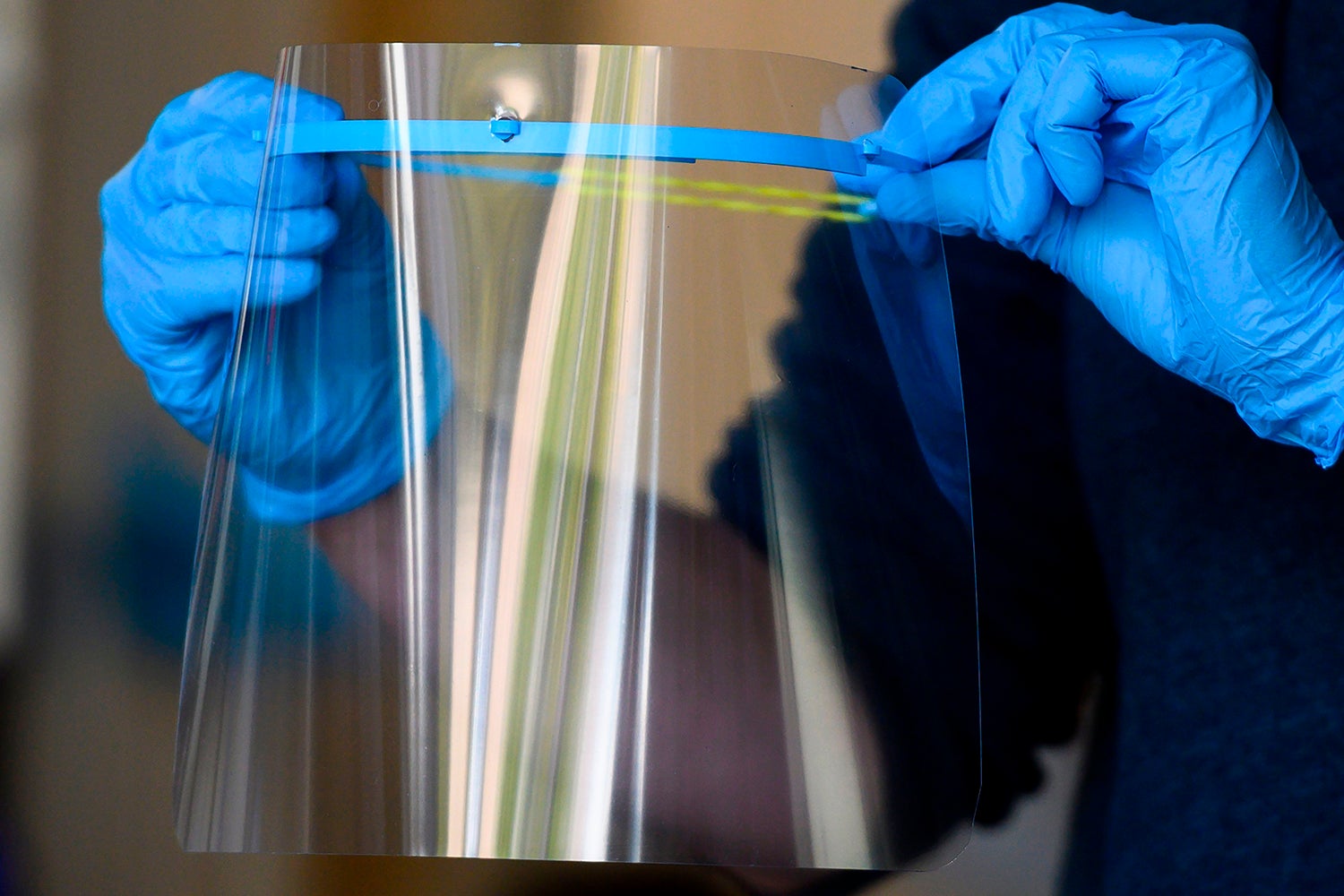
But masks are only just one element of the particular protecting equipment that wellness treatment employees need—and they do not demand a redesign for stitching machines to manufacture them en masse. Gear this sort of as encounter shields—transparent plastic sheets that wearers strap to their brow to offer an extra barrier versus droplets—are another story. It is achievable to MacGyver this sort of a system from a sheet of plastic and zip ties or rubber bands, but the procedure and final results would be far too time-consuming and unwell-fitting for mass output. Instead engineers have appear up with many ways to make facial shields that 3-D printers and laser cutters can churn out.
Facial Security
Bhamla is a member of just one of the to start with groups using a Do-it-yourself method to coronavirus equipment, which is coordinated on the business interaction system Slack. When Nicholas Moser to start with joined the team, termed Useful Engineering, he says it had roughly three hundred individuals. As its aim shifted to coronavirus-combating types, membership ballooned to countless numbers at the time of this composing. Moser, who has expertise as a undertaking supervisor, turned guide of MASKproject, a subgroup that aims to establish protecting gear. MASKproject immediately began refining two encounter shields, eventually focusing on an origami-type style and design. Any commercial die cutter, laser cutter or h2o jet can slice the open-supply style and design from a flat sheet of plastic, which is then folded by hand into the correct three-dimensional shape.
Moser says his team’s encounter shields are currently heading out to 5 hospitals, including types in New Orleans, Massachusetts and California, at a fee of about 10,000 for each 7 days. Other businesses have adopted: equally the Massachusetts Institute of Engineering and Duke University Overall health Process have announced that their researchers developed and examined their have encounter-shield prototypes. Like the MASKproject’s style and design, M.I.T.’s shield is produced on a die-chopping device and then folded by hand, whilst Duke Health’s works by using a 3-D-printed headband.
In all these conditions, the new shields can be produced on rather frequent machines—laser cutters, die cutters and 3-D printers are identified in numerous maker areas, labs and output amenities that do not generally make healthcare equipment. Moser’s workforce wants to perform with a range of associates to develop its equipment, he says. “Everything from a small store that does letterpress—that cuts out items of paper in shapes—to substantial factories that have roller die cutters that can develop hundreds of countless numbers [of shields] a working day,” Moser provides. Products churned out by this so-termed distributed-producing product then flow to a central hub for good quality control and sanitization just before they are transported to hospitals. “Part of this undertaking, which is fascinating, is that there’s in no way been this type of distributed producing,” he says. “This scale of distributed producing has in no way been done. And the offer chains are acquiring worked out astonishingly swiftly, with all these persons.”
In Need of N95s
Despite the fact that distributed producing has the benefit of velocity, it needs reengineering equipment so that merchandise can be produced with machines this sort of as 3-D printers somewhat than specialised equipment. And not all the new types fulfill rigorous healthcare requirements, which are especially important for key merchandise that are now seriously scarce: N95 respirators. Surgical masks can halt droplets, but viruses can nevertheless squeeze by the substance. This probability is a issue when the air will get filled with viral particles, which happens when physicians ventilate seriously unwell coronavirus clients. To protect themselves in this sort of conditions, healthcare pros don N95 respirators. These masks healthy snugly to the pores and skin, only admitting air by a dense filter that blocks 95 % of really small particles when nevertheless allowing wearers to breathe with out undue effort.
The filter inside of an N95 is manufactured of spun polypropylene, a substance currently in short offer. So Moser and his colleagues are designing a similar system that can utilize other substances. “We have made and prototyped and are testing a filter-agnostic encounter shield to be an alternate to N95,” he says. The MASKproject respirator is composed of a 3-D-printed base that can healthy tightly to the encounter. The products has a front grate that forces air to enter by a stack of filtering components, including high-performance particulate air filters “that fulfill the identical particle specification as the N95. So they are not rated for being utilised like this, but they have a similar classification,” Moser says. His team is currently testing the equipment for equally filtering and breathability.
MASKproject’s system is not likely to bounce by all the regulatory hoops that accredited N95 respirators will have to go, having said that. “Products like N95 respirators do go by a stringent testing procedure to be capable at that degree,” says Julie Swann, a professor of industrial and methods engineering at North Carolina State University. But the latest pandemic will not wait around for testing: the Foodstuff and Drug Administration not too long ago announced that in unexpected emergency conditions, U.S. businesses can convert to substitutes this sort of as KN95s, comparable protectors utilised in China. Moser sees his team’s alternate to N95 as a similar backup possibility. “MASKproject, myself and Useful Engineers—we’re not earning healthcare equipment,” he says. “We’re earning common-use products that we are testing to the identical international requirements as the comparable equipment that are in short offer. But they are not accredited, and they are not controlled, and they are not intended for healthcare use.” Moser notes that hospitals can request MASKproject’s equipment, “but they are not being marketed for healthcare use at all.” Despite this disclaimer, he says, his workforce is pursuing certification from the Fda and the Countrywide Institute for Occupational Basic safety and Overall health at the U.S. Facilities for Sickness Regulate and Avoidance.
Ventilator Redesign
Like N95 respirators, ventilators will have to fulfill particularly rigorous requirements. When the amount of oxygen in COVID-19 patients’ blood drops to harmful stages, these machines try to breathe for them. But the sophisticated, costly equipment are in constrained offer all around the globe, even as manufacturers increase their fee of output.
“In the U.K., the difficulty is that our ventilator manufacturers are fantastic—but latest capacity to manufacture is about 2,000 for each 12 months,” says Mark Thompson, an engineer at the University of Oxford. He notes that the state will require numerous much more machines than that in get to guidance the estimated quantity of COVID-19 clients who will demand them in the coming months. “It’s just not achievable to scale the output of any just one of our ventilator manufacturers,” he says. “It requires to have a fully unique remedy.”
Thompson is just one of many researchers spearheading the enhancement of a single-use ventilator substitute motivated by an current products: the squeeze bag that wellness employees utilize to manually control a patient’s respiratory in unexpected emergency conditions. With an oxygen offer and an apparatus to automate the squeeze-and-release procedure, this sort of a system could help an contaminated individual breathe for a extended interval of time in a way similar to a ventilator. In this situation, Thompson’s workforce required to attain that automated procedure with off-the-shelf elements to make the system a lot easier to manufacture. “Essentially, it revolves all around this idea of having lots of single-use merchandise [that] are greatly out there [and that] are all affected person-struggling with items of equipment,” he says. Just after a breakneck two-7 days enhancement interval, Thompson and his colleagues began testing their ventilator substitute, termed OxVent. And they are currently in the second spherical of testing to secure acceptance from the Medications and Health care Solutions Regulatory Company, a U.K. entire body akin to the Fda in the U.S. As soon as the builders get the inexperienced light-weight, they system to have healthcare system company Smith+Nephew develop their open-supply style and design.
OxVent was an early entry in the race to redesign ventilators for speedier producing, but it is not the only contender. A few unique groups of physicists have developed their have unexpected emergency ventilator prototypes. And this month the CoVent-19 Challenge released an open contest contacting for new ventilator types. The system is that they will be developed around the system of only two months.
These types will not be as advanced as normal ventilators. For instance, Thompson notes that his team’s products will have to be discarded just after it is utilised on a single affected person. It will also deficiency the checking equipment and alarms that whole-scale ventilators have. On the other hand, organizations will be in a position to scale up output of unexpected emergency ventilator types a lot much more immediately by working with the sort of distributed producing that Moser’s perform also relies on. “The challenge is to [make] an extra quantity of about twenty,000 ventilators just before the peak of the epidemic,” Thompson says. “We feel that with that kind of distributed procedure, we have a chance of running to do that.”
Go through much more about the coronavirus outbreak here.





