Metabolic mutations help bacteria resist drug treatment | MIT News
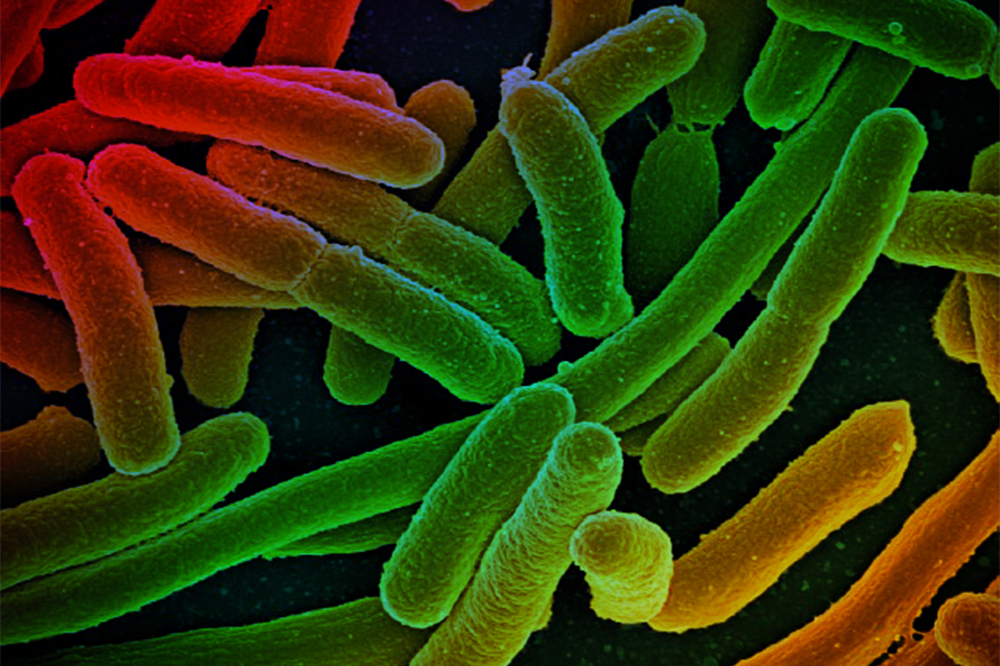
Bacteria have many approaches to evade the antibiotics that we use in opposition to them. Every single yr, at minimum 2.8 million persons in the United States build an antibiotic-resistant an infection, and a lot more than 35,000 men and women die from this sort of infections, according to the U.S. Facilities for Disorder Command.
Most of the mutations identified to confer resistance happen in the genes qualified by a distinct antibiotic. Other resistance mutations permit microorganisms to crack down antibiotics or pump them out via their mobile membranes.
MIT researchers have now discovered an additional class of mutations that helps microbes produce resistance. In a analyze of E. coli, they uncovered that mutations to genes associated in metabolism can also assist microbes to evade the toxic effects of quite a few different antibiotics. The findings drop mild on a fundamental side of how antibiotics perform, and suggest prospective new avenues for producing medicine that could boost the usefulness of current antibiotics, the scientists say.
“This examine offers us insights into how we can enhance the efficiency of present antibiotics mainly because it emphasizes that downstream metabolic process performs an vital role. Specifically, our perform implies that the killing efficacy of an antibiotic can be increased if 1 can elevate the metabolic response of the taken care of pathogen,” says James Collins, the Termeer Professor of Healthcare Engineering and Science in MIT’s Institute for Clinical Engineering and Science (IMES) and Section of Biological Engineering.
Collins is the senior author of the review, which seems right now in Science. The paper’s direct creator is Allison Lopatkin, a former MIT postdoc who is now an assistant professor of computational biology at Barnard School at Columbia University.
Metabolic control
The new review builds on prior perform from Collins’ lab demonstrating that when addressed with antibiotics, numerous bacteria are forced to ramp up their metabolic process, primary to an accumulation of poisonous byproducts. These byproducts harm the cells and contribute to their dying.
Nonetheless, even with the position of overactive metabolic rate in cell loss of life, experts had not discovered any proof that this metabolic pressure sales opportunities to mutations that assist bacteria evade the prescription drugs. Collins and Lopatkin established out to see if they could locate this sort of mutations.
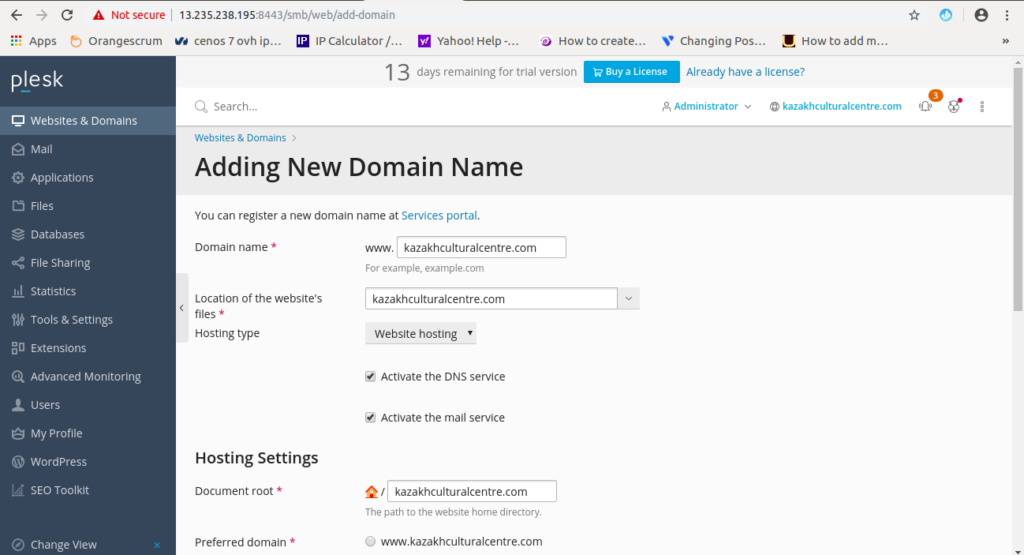
1st, they done a examine similar to people commonly applied to seem for antibiotic resistance mutations. In this variety of screen, recognized as adaptive evolution, scientists begin with a laboratory pressure of E. coli and then treat the cells with progressively increasing doses of a individual antibiotic. Scientists then sequence the cells’ genomes to see what kinds of mutations arose through the study course of the procedure. This technique has not formerly yielded mutations to genes involved in metabolism, due to the fact of restrictions in the quantity of genes that could be sequenced.
“Many of the scientific studies before now have looked at a couple unique advanced clones, or they sequence maybe a couple of the genes the place we anticipate to see mutations simply because they’re related to how the drug functions,” Lopatkin suggests. “That gives us a pretty precise photo of all those resistance genes, but it boundaries our perspective of everything else that’s there.”
For instance, the antibiotic ciprofloxacin targets DNA gyrase, an enzyme included in DNA replication, and forces the enzyme to injury cells’ DNA. When treated with ciprofloxacin, cells frequently produce mutations in the gene for DNA gyrase that allow them to evade this system.
In their initial adaptive evolution monitor, the MIT group analyzed much more E. coli cells and quite a few much more genes than had been researched just before. This authorized them to recognize mutations in 24 metabolic genes, such as genes relevant to amino acid metabolic process and the carbon cycle — the established of chemical reactions that enables cells to extract electricity from sugar, releasing carbon dioxide as a byproduct.
To tease out even far more fat burning capacity-relevant mutations, the scientists ran a 2nd display in which they compelled the cells into a heightened metabolic state. In these reports, E. coli have been taken care of with a high focus of an antibiotic every working day, at incrementally rising temperatures. The temperature modifications slowly drove the cells into a quite active metabolic state, and at the very same time, they also progressively progressed resistance to the drug.
The scientists then sequenced the genomes of these micro organism and uncovered some of the very same rate of metabolism-similar mutations they saw in the initial display, in addition extra mutations to fat burning capacity genes. These bundled genes concerned in synthesis of amino acids, specially glutamate, in addition to the carbon cycle genes. They then in contrast their benefits to a library of genomes of resistant microbes isolated from individuals, and observed several of the very same mutations.
New targets
The scientists then engineered some of these mutations into regular E. coli strains and located that their premiums of mobile respiration ended up significantly diminished. When they taken care of these cells with antibiotics, much much larger doses had been needed to destroy the germs. This implies that by turning down their metabolic process just after drug treatment method, microbes can stop the buildup of dangerous byproducts.
The findings raise the risk that forcing germs into a heightened metabolic condition could improve the success of existing antibiotics, the researchers say. They now system to further more examine how these metabolic mutations enable microbes evade antibiotics, in hopes of identifying more specific targets for new adjuvant medicines.
“I feel these final results are definitely interesting due to the fact it unleashes gene targets that could boost antibiotic efficacy, that are not being now investigated,” Lopatkin says. “New resistance mechanisms are actually enjoyable simply because they give numerous new avenues of investigation to observe up on and to see to what extent is this heading to boost the efficacy for dealing with clinical strains.”
The research was funded by the Protection Danger Reduction Company, the Countrywide Institutes of Wellness, the National Science Basis Graduate Investigation Fellowship Program, the Broad Institute of MIT and Harvard, and a gift from Anita and Josh Bekenstein.