Method for delivering immune system-stimulating drugs may enhance cancer immunotherapy | MIT News
Stimulating the body’s immune method to assault tumors is a promising way to treat cancer. Researchers are doing the job on two complementary techniques to realize that: having off the brakes that tumors put on the immune technique and “stepping on the fuel,” or offering molecules that jumpstart immune cells.
Nevertheless, when jumpstarting the immune system, scientists have to be thorough not to overstimulate it, which can lead to significant and perhaps deadly side results. A workforce of MIT scientists has now made a new way to deliver a stimulatory molecule referred to as IL-12 directly to tumors, steering clear of the toxic consequences that can occur when immunostimulatory medicines are supplied through the overall body.
In a analyze of mice, this new treatment removed numerous tumors when delivered together with an Food and drug administration-permitted drug that can take the brakes off the immune program.
“Even past this particular scenario of IL-12, which we seriously hope will have some impact, it is a approach that you could use to any of these immunostimulatory drugs,” says Darrell Irvine, who is the Underwood-Prescott Professor with appointments in MIT’s departments of Biological Engineering and Supplies Science and Engineering an associate director of MIT’s Koch Institute for Integrative Cancer Research and a member of the Ragon Institute of MGH, MIT, and Harvard.
The scientists have submitted for patents on their technique, and the engineering has been accredited to a startup that hopes to get started clinical trials by the close of 2022.
Irvine and Dane Wittrup, the Carbon P. Dubbs Professor of Chemical Engineering and Electrical Engineering and a member of the Koch Institute, are the senior authors of the analyze, which seems nowadays in Character Biomedical Engineering. MIT graduate pupil Yash Agarwal is the paper’s guide creator.
Stepping on the gas
As tumors produce, they secrete molecules that disable close by T cells and other immune cells, allowing the tumors to develop unchecked. Prescription drugs recognised as checkpoint blockade inhibitors, which can acquire these brakes off the immune program, are now utilized to treat some forms of cancer, but a lot of other kinds are resistant to this form of remedy.
Combining checkpoint inhibitors with prescription drugs that encourage the immune procedure could probably make cancer immunotherapy function for additional individuals. Cytokines, which are immune substances in a natural way manufactured by the entire body, are one particular class of medication that scientists have experimented with as a way to “step on the fuel.” However, in clinical trials, these drugs have shown far too lots of toxic facet results, ranging from flu-like indicators to organ failure.
“If you soak the affected individual in cytokines, their entire system reacts and you get such a robust, harmful facet influence that you simply cannot achieve the amounts you want you could in the tumor and get the effects that you want,” Wittrup states.
To consider to stay away from individuals facet effects, Wittrup and Irvine have been doing work on means to produce cytokines in a a lot more specific way. In a 2019 analyze, they confirmed that they could supply the cytokines IL-12 and IL-2 immediately to tumors by attaching the cytokines to a collagen-binding protein. This protein then sticks to collagen observed in tumors, which commonly have massive quantities of collagen.
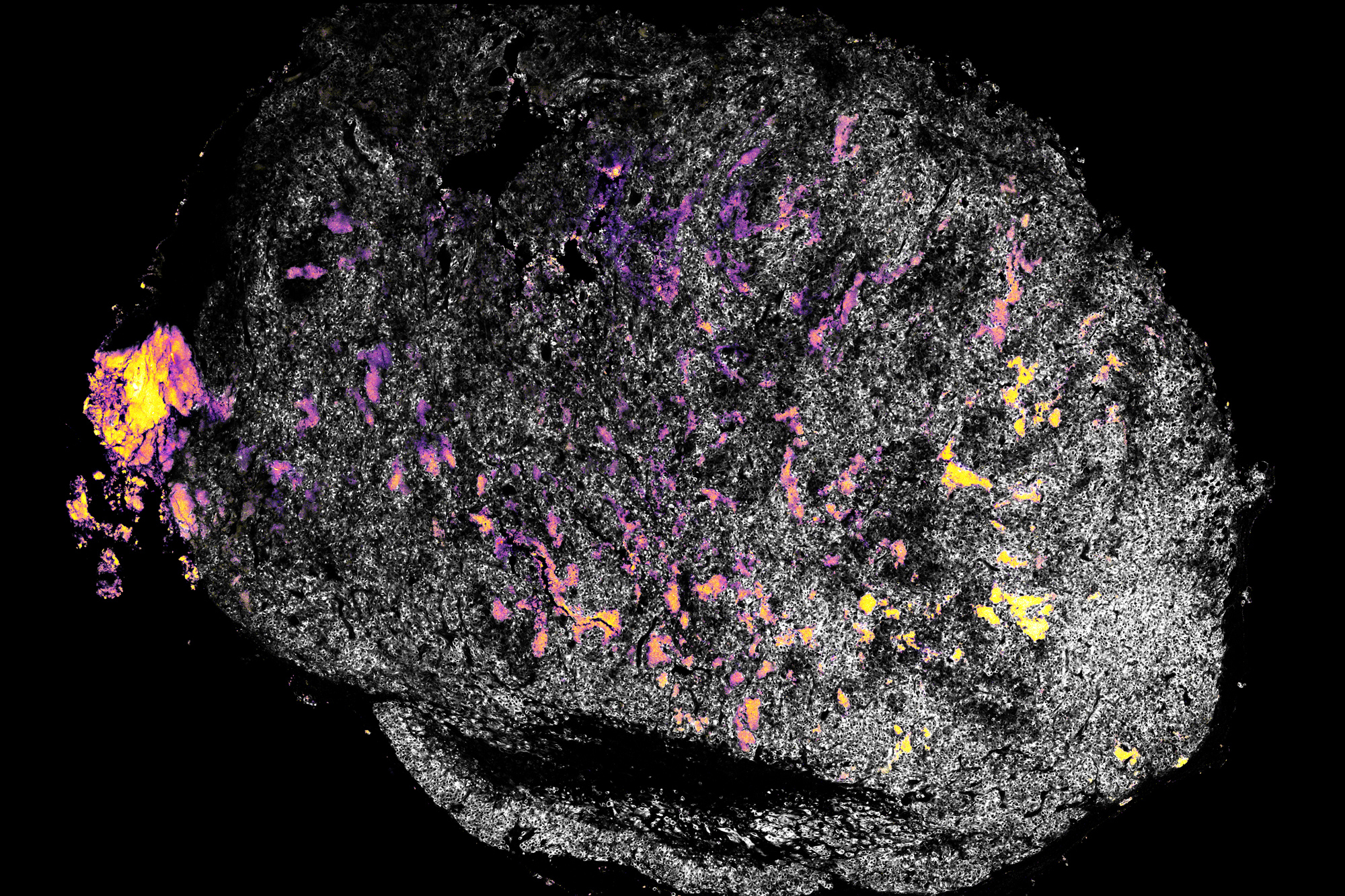
This system labored properly in a study of mice, but the researchers needed to uncover a way to make cytokines bind even far more strongly to tumors. In their new analyze, they replaced the collagen-binding protein with aluminum hydroxide. This compound, also referred to as alum, is typically applied as a vaccine adjuvant (a drug that assists strengthen the immune response to vaccination).
“One key advantage of alum is that the particles are on the micron measurement scale, so when you inject them in folks or in mice, they continue to be wherever you inject them for weeks, going on to months occasionally,” Agarwal suggests.
Fighting tumors
To take a look at the effectiveness of this remedy, the scientists gave mice a person injection of IL-12 or IL-2 certain to alum particles, and addressed the mice with a checkpoint blockade inhibitor identified as anti-PD1 each handful of days.
In mouse designs of 3 forms of most cancers, the researchers observed that the tumors have been removed in 50 to 90 per cent of the mice. In a design where breast most cancers cells were transplanted into mice, and then metastasized to the lungs, one injection at the breast most cancers site also cleared the metastatic tumors, even while IL-12 was not injected into the lungs.
Alum-IL-12 particles supplied without the checkpoint blockade inhibitors also confirmed some ability to promote the immune method to battle tumors.
Even further experiments confirmed that IL-12 stimulates the manufacturing of an additional cytokine referred to as interferon gamma, and these two molecules function together to activate T cells as effectively as dendritic cells and macrophages. The procedure also stimulates memory T cells that may possibly be ready to respond to tumors that regrow.
The scientists also observed that the handled mice did not demonstrate any of the side results that are viewed when IL-12 is given systemically. The startup firm that has certified the technological innovation plans to initially examination IL-12-alum particles on their very own, and if that cure is proven to be harmless, they hope to check Il-12 in blend with checkpoint blockade inhibitors.
The new solution of attaching molecules to alum could also be employed to deliver other varieties of immunostimulatory medicines, the researchers say.
“This total class of medicines that entails stepping on the fuel has largely not succeeded nevertheless. Our hope is that this opens the way to take a look at any of all those medicines,” Irvine says.
The exploration was funded in section by the Koch Institute’s Marble Centre for Nanomedicine the Ragon Institute of MGH, MIT and Harvard and the Koch Institute Aid (core) Grant from the National Most cancers Institute.

