Our gut-brain connection | MIT News
In many strategies, our mind and our digestive tract are deeply connected. Experience anxious may possibly lead to physical agony in the belly, even though hunger indicators from the intestine make us feel irritable. Modern research have even prompt that the bacteria residing in our gut can impact some neurological disorders.
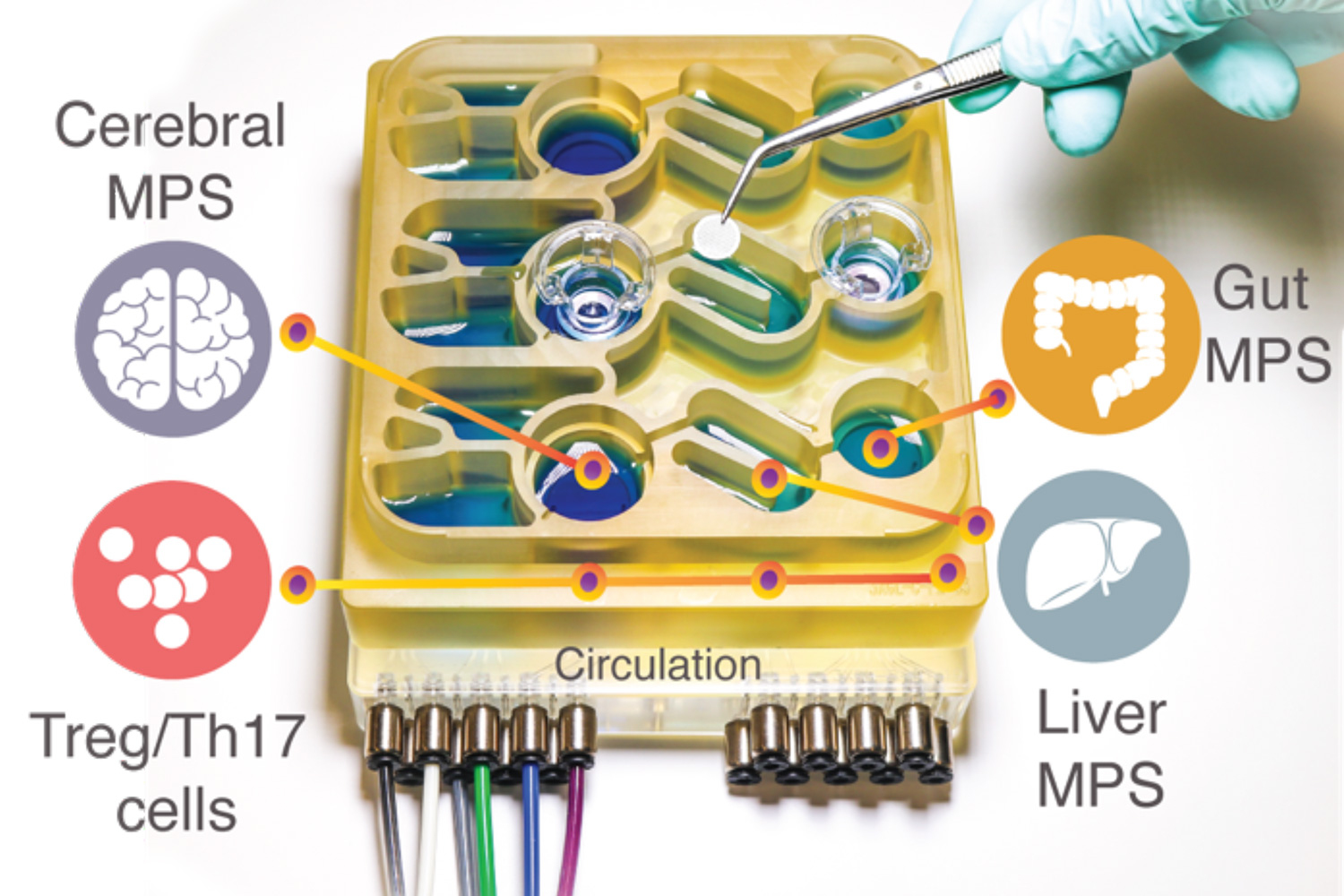
Modeling these intricate interactions in animals such as mice is complicated to do, since their physiology is quite unique from humans’. To enable researchers improved understand the intestine-brain axis, MIT researchers have developed an “organs-on-a-chip” method that replicates interactions concerning the mind, liver, and colon.
Using that program, the scientists were equipped to product the influence that microbes dwelling in the intestine have on both of those nutritious mind tissue and tissue samples derived from sufferers with Parkinson’s sickness. They observed that limited-chain fatty acids, which are produced by microbes in the intestine and are transported to the brain, can have incredibly various consequences on balanced and diseased brain cells.
“While quick-chain fatty acids are largely useful to human overall health, we noticed that below selected ailments they can even more exacerbate specified brain pathologies, these types of as protein misfolding and neuronal loss of life, relevant to Parkinson’s condition,” claims Martin Trapecar, an MIT postdoc and the guide author of the review.
Linda Griffith, the College of Engineering Professor of Teaching Innovation and a professor of organic engineering and mechanical engineering, and Rudolf Jaenisch, an MIT professor of biology and a member of MIT’s Whitehead Institute for Professional medical Investigation, are the senior authors of the paper, which appears right now in Science Advancements.
The intestine-mind link
For numerous a long time, Griffith’s lab has been establishing microphysiological methods — modest gadgets that can be utilised to develop engineered tissue products of different organs, related by microfluidic channels. In some conditions, these products can provide much more correct facts on human ailment than animal types can, Griffith claims.
In a paper released final year, Griffith and Trapecar applied a microphysiological method to product interactions between the liver and the colon. In that analyze, they observed that short-chain fatty acids (SCFAs), molecules created by microbes in the intestine, can worsen autoimmune inflammation linked with ulcerative colitis beneath selected conditions. SCFAs, which include things like butyrate, propionate, and acetate, can also have advantageous results on tissues, which includes amplified immune tolerance, and they account for about 10 % of the electricity that we get from food items.
In the new study, the MIT group decided to include the mind and circulating immune cells to their multiorgan technique. The mind has several interactions with the digestive tract, which can come about by means of the enteric anxious program or via the circulation of immune cells, vitamins, and hormones between organs.
Quite a few years ago, Sarkis Mazmanian, a professor of microbiology at Caltech, learned a connection in between SCFAs and Parkinson’s disorder in mice. He confirmed that SCFAs, which are made by microbes as they consume undigested fiber in the gut, sped up the progression of the condition, though mice lifted in a germ-no cost setting ended up slower to develop the illness.
Griffith and Trapecar determined to even more check out Mazmanian’s results, making use of their microphysiological model. To do that, they teamed up with Jaenisch’s lab at the Whitehead Institute. Jaenisch experienced formerly developed a way to transform fibroblast cells from Parkinson’s patients into pluripotent stem cells, which can then be induced to differentiate into unique types of mind cells — neurons, astrocytes, and microglia.
Far more than 80 % of Parkinson’s scenarios simply cannot be joined to a certain gene mutation, but the relaxation do have a genetic trigger. The cells that the MIT scientists applied for their Parkinson’s product have a mutation that results in accumulation of a protein called alpha synuclein, which damages neurons and triggers inflammation in brain cells. Jaenisch’s lab has also generated brain cells that have this mutation corrected but are if not genetically equivalent and from the same affected individual as the diseased cells.
Griffith and Trapecar first examined these two sets of mind cells in microphysiological methods that ended up not related to any other tissues, and uncovered that the Parkinson’s cells confirmed far more irritation than the healthful, corrected cells. The Parkinson’s cells also had impairments in their means to metabolize lipids and cholesterol.
Reverse consequences
The researchers then related the brain cells to tissue styles of the colon and liver, utilizing channels that let immune cells and nutrients, like SCFAs, to movement among them. They discovered that for balanced mind cells, staying uncovered to SCFAs is valuable, and can help them to experienced. However, when brain cells derived from Parkinson’s sufferers had been exposed to SCFAs, the effective effects disappeared. As a substitute, the cells knowledgeable increased ranges of protein misfolding and cell death.
These outcomes had been noticed even when immune cells were taken off from the procedure, foremost the scientists to hypothesize that the effects are mediated by variations to lipid metabolic process.
“It appears to be that short-chain fatty acids can be joined to neurodegenerative ailments by affecting lipid metabolic rate rather than specifically impacting a specific immune mobile populace,” Trapecar claims. “Now the target for us is to check out to realize this.”
The researchers also approach to design other styles of neurological conditions that may possibly be influenced by the intestine microbiome. The conclusions present assistance for the notion that human tissue versions could generate facts that animal products simply cannot, Griffith says. She is now doing the job on a new version of the model that will include micro blood vessels connecting distinctive tissue types, allowing scientists to review how blood circulation between tissues influences them.
“We must be genuinely pushing enhancement of these, mainly because it is important to begin bringing more human features into our products,” Griffith states. “We have been able to start out obtaining insights into the human issue that are tricky to get from mice.”
The study was funded by DARPA, the National Institutes of Health and fitness, the Countrywide Institute of Biomedical Imaging and Bioengineering, the National Institute of Environmental Health Sciences, the Koch Institute Support (core) Grant from the National Cancer Institute, and the Military Investigate Business office Institute for Collaborative Biotechnologies.

