Weighing cancer cells to personalize drug choices | MIT News
Scientists at MIT and Dana-Farber Most cancers Institute have produced a new way to ascertain regardless of whether personal people will reply to a precise most cancers drug or not. This sort of check could support health professionals to pick out alternate therapies for clients who don’t answer to the therapies normally used to deal with their cancer.
The new system, which involves getting rid of tumor cells from individuals, treating the cells with a drug, and then measuring alterations in the cells’ mass, could be utilized to a extensive variety of cancers and drug treatments, says Scott Manalis, the David H. Koch Professor of Engineering in the departments of Organic Engineering and Mechanical Engineering, and a member of the Koch Institute for Integrative Most cancers Analysis.
“Essentially all of the clinically utilized cancer drugs possibly immediately or indirectly end the expansion of most cancers cells,” Manalis suggests. “That’s why we imagine measuring mass could offer you a common readout of the results of a ton of diverse varieties of drug mechanisms.”
The new review, which focused on glioblastoma, an aggressive sort of mind most cancers, is component of a collaboration involving the Koch Institute and Dana-Farber Precision Drugs systems to find new biomarkers and diagnostic exams for most cancers.
Manalis and Keith Ligon, director of the Center for Patient Derived Products at Dana-Farber and an associate professor at Harvard Healthcare University, are the senior authors of the analyze, which seems right now in Cell Experiences. The guide authors of the paper are Max Stockslager SM ’17, PhD ’20 and Dana-Farber research technician Seth Malinowski.
Measuring most cancers cells
Glioblastoma, which is diagnosed in about 13,000 Americans for each yr, is incurable, but radiation and drug therapy can enable to lengthen patients’ anticipated lifespan. Most do not survive more time than one particular to two decades.
“With this disorder, you do not have substantially time to make changes. So, if you choose an ineffective drug for 6 months, which is fairly sizeable,” Ligon suggests. “This form of assay could aid to speed up the studying system for just about every unique individual and support with final decision-making.”
Individuals diagnosed with glioblastoma are usually specified a chemotherapy drug called temozolomide (TMZ). Nevertheless, this drug only assists about 50 % of patients.
At present doctors can use a genetic marker — methylation of a gene termed MGMT — to predict irrespective of whether people will react to TMZ remedy. Clients who have this marker typically reply superior to the drug. Nonetheless, the marker does not supply trusted predictions for all sufferers because of other genetic elements. For people who do not respond to TMZ, there are a handful of different medication obtainable, Ligon states, or clients can opt for to participate in a scientific trial.
In the latest many years, Manalis and Ligon have been doing work on a new technique to predicting individual responses, which is dependent on measuring how tumor cells react to remedy, rather than genomic signatures. This strategy is recognised as useful precision drugs.
“The plan powering practical precision drugs is that, for cancer, you could acquire a patient’s tumor cells, give them the medicines that the affected person might get, and predict what would occur, prior to giving them to the affected person,” Ligon claims.
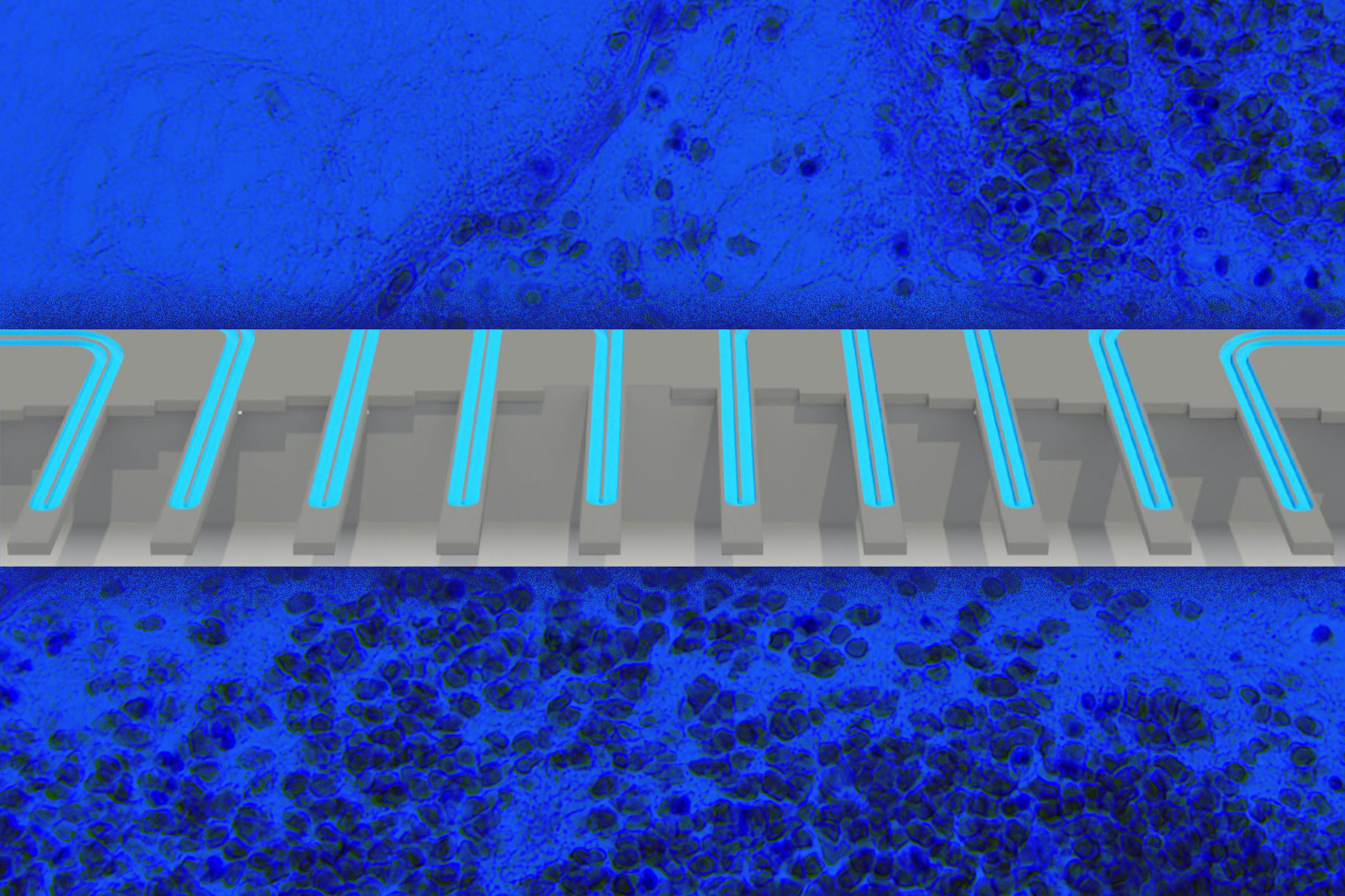
Scientists are performing on several diverse approaches to purposeful precision medicine, and one technique that Manalis and Ligon have been pursuing is measuring improvements in mobile mass that happen next drug treatment method. The tactic is primarily based on a technology produced by Manalis’ lab for weighing solitary cells with particularly high accuracy by flowing them by vibrating microchannels.
Various yrs back, Manalis, Ligon, and their colleagues shown that they could use this technologies to review how two forms of cancer, glioblastoma and acute lymphoblastic leukemia, answer to treatment. This result was primarily based on measuring unique cells many instances following drug therapy, making it possible for the scientists to work out how their growth level modified about time subsequent remedy. They showed that this statistic, which they referred to as mass accumulation charge (MAR), was strongly predictive of whether or not the cells were inclined to a specified drug.
Using a substantial-throughput edition of this method, which they produced in 2016, they could determine an exact MAR employing just 100 cells for every individual. Nonetheless, a drawback to the MAR strategy is that the cells should continue to be in the process for quite a few hours, so they can be weighed about and over, in order to determine the advancement rate in excess of time.
In their new review, the scientists decided to see if a less difficult and substantially quicker approach — measuring subtle modifications in one-cell mass distributions concerning drug-dealt with and untreated most cancers cells — would be in a position to forecast individual survival. They done a retrospective study with a established of stay glioblastoma tumor cells from 69 clients, donated to the Ligon lab and the Dana-Farber Middle for Affected person Derived Versions, and utilised them to improve spheroid tissue cultures. Immediately after separating the cells, the scientists handled them with TMZ and then calculated their mass a several times later on.
They found that by only measuring the mass change between cells in advance of and following cure, working with as couple of as 2,000 cells per individual sample, they could correctly forecast no matter whether the patient experienced responded to TMZ or not.
Greater predictions
The scientists showed that their mass measurement was just as accurate as the MGMT methylation marker, but mass measurement has an extra edge in that it can work in patients for whom the genetic marker doesn’t reveal TMZ susceptibility. For quite a few other kinds of cancer, there are no biomarkers that can be utilised to predict drug reaction.
“Most cancers do not have a genomic marker that can be utilised at all. What we argue is that this functional approach could perform in other conditions exactly where you don’t have any selection of a genomic marker,” Manalis says.
For the reason that the test is effective by measuring changes in mass, it can be applied to notice the effects of quite a few distinctive styles of most cancers medication, irrespective of their mechanism of motion. TMZ works by arresting the cell cycle, which results in cells to become larger sized due to the fact they can no extended divide but they even now increase their mass. Other cancer prescription drugs perform by interfering with mobile metabolic process or harmful their composition, which also affect cell mass.
The researchers’ prolonged-time period hope is that this technique could be made use of to take a look at many diverse medicine on an particular person patient’s cells, to forecast which therapy would operate ideal for that affected individual.
“Ideally we would check the drug the affected individual was most probably to get, but we would also check for issues that would be the backup plan: first-, second-, and 3rd-line therapies, or distinctive combos of medications,” states Ligon, who also serves as chief of neuropathology at the Brigham and Women’s Healthcare facility and a consultant in pathology at Boston Children’s Clinic.
Manalis and Ligon have co-founded a firm referred to as Travera, which has licensed this technological innovation and is now accumulating knowledge from patient samples from numerous unique types of most cancers, in hopes of acquiring clinically validated lab assessments that can be used to support clients.
The investigation was funded by the MIT Centre for Precision Cancer Medicine, the DFCI Middle for Affected individual Derived Styles, the Cancer Methods Biology Consortium of the National Cancer Institute, and the Koch Institute Assistance (main) Grant from the National Most cancers Institute.




